In today’s patient-centred healthcare landscape, measuring and understanding patient experience and satisfaction have become crucial for healthcare organizations striving to deliver high-quality care.
Patient experience encompasses all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care (LaVela & Gallan, 2014). By systematically collecting and analysing patient feedback, healthcare providers can identify areas for improvement, make informed decisions, and enhance the overall quality of care.
Measuring patient experience and satisfaction offers several key benefits:
- Identifies opportunities for quality improvement initiatives
- Helps prioritize resource allocation and service enhancements
- Facilitates benchmarking and comparative performance assessment
- Promotes patient engagement and empowerment
- Supports compliance with regulatory and accreditation requirements
As healthcare organizations increasingly recognize the value of patient experience feedback, various tools and methodologies have emerged to capture and measure these critical aspects of care delivery.
- Understanding Patient Experience and Satisfaction
- Net Promoter Score (NPS) and the Friends and Family Test (FFT)
- Implementing NPS/FFT in Health Care Settings
- Lessons learned and best practices for using NPS/FFT effectively
- Integrating NPS/FFT with Other Patient Experience Measures
- Future Directions and Challenges
- References
Understanding Patient Experience and Satisfaction
Defining patient experience and its key elements
Patient experience is a multifaceted concept that encompasses all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care (Wolf et al., 2014).
It goes beyond simple measures of patient satisfaction and includes various aspects of care delivery, such as communication, empathy, and responsiveness to individual needs and preferences.
Key elements of patient experience include:
- Interpersonal aspects of care (e.g., communication, empathy, and respect)
- Technical aspects of care (e.g., clinical competence and safety)
- Accessibility and convenience (e.g., wait times and ease of navigation)
- Physical environment (e.g., cleanliness, comfort, and amenities)
- Continuity and coordination of care
- Emotional support and alleviation of fear and anxiety
- Involvement of family and friends
- Information, communication, and education
Understanding and addressing these elements is crucial for healthcare organizations seeking to improve patient experience and deliver patient-centred care.
The evolution of measuring patient satisfaction
The measurement of patient satisfaction in healthcare has evolved significantly over the past few decades. Early efforts focused primarily on simple, post-discharge surveys that assessed overall satisfaction with care. However, these measures often lacked specificity and failed to capture the nuances of patient experiences (Kash & McKahan, 2017).
In the 1980s and 1990s, the development of standardized survey instruments, such as the Press Ganey Patient Satisfaction Survey and the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), marked a significant advancement in patient satisfaction measurement.
These tools provided more comprehensive and comparable data on specific aspects of care, such as communication with doctors and nurses, pain management, and discharge information.
More recently, the focus has shifted toward a broader understanding of patient experience, recognizing the importance of capturing patient perceptions and emotions throughout the entire care journey.
This has led to the adoption of real-time feedback mechanisms, qualitative methods (e.g., patient interviews and focus groups), and the integration of patient experience data with other quality and safety metrics.
The relationship between patient experience, satisfaction, and quality of care
Patient experience, satisfaction, and quality of care are closely interrelated concepts in healthcare.
A positive patient experience is often associated with higher levels of satisfaction, which in turn can influence patient engagement, adherence to treatment plans, and overall health outcomes.
Studies have demonstrated that patient experience measures, such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, are positively correlated with clinical quality indicators, such as adherence to evidence-based practices and lower hospital readmission rates (Manary et al., 2013).
This suggests that healthcare organizations that prioritize patient experience and satisfaction are more likely to deliver high-quality care.
However, it is important to note that patient satisfaction alone does not necessarily equate to high-quality care.
In some cases, patients may express satisfaction with suboptimal care, or conversely, may be dissatisfied with clinically appropriate care that challenges their preferences or expectations.
Therefore, healthcare organizations must strive to balance patient experience and satisfaction with evidence-based practices and clinical expertise to ensure the delivery of safe, effective, and patient-centred care.
By understanding the complex relationship between patient experience, satisfaction, and quality of care, healthcare leaders can develop comprehensive strategies to measure, monitor, and improve these critical aspects of healthcare delivery.
Net Promoter Score (NPS) and the Friends and Family Test (FFT)
Introduction to NPS and its application in various industries
The Net Promoter Score (NPS) is a widely used metric for gauging customer loyalty and satisfaction, originally developed by Fred Reichheld and Bain & Company.
The NPS is based on a single question:
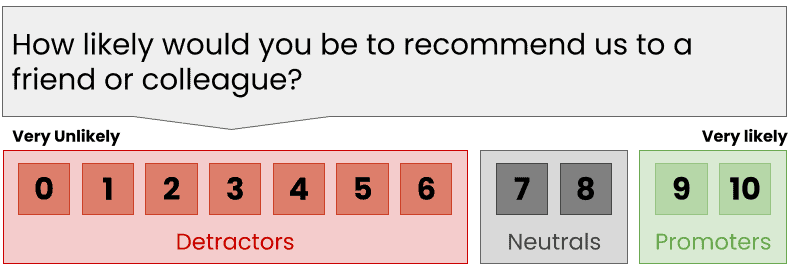
Respondents are categorized into Promoters (9-10), Passives (7-8), and Detractors (0-6), and the NPS is calculated by subtracting the percentage of Detractors from the percentage of Promoters.
NPS has been adopted across various industries, including telecommunications, banking, retail, and hospitality. Companies use NPS to track customer loyalty over time, benchmark against competitors, and identify opportunities for improvement.
The simplicity and ease of implementation of NPS have contributed to its widespread adoption as a customer feedback metric.
Adapting NPS to health care settings: The Friends and Family Test (FFT)
In recent years, healthcare organizations have recognized the potential of NPS to measure patient satisfaction and loyalty.
The Friends and Family Test (FFT) is an adaptation of NPS specifically designed for healthcare settings. The FFT asks patients,
How likely are you to recommend our [ward/service/organization] to your friends and family if they needed similar care or treatment?
The FFT has been implemented in various healthcare systems worldwide, most notably in the United Kingdom’s National Health Service (NHS). The NHS has mandated the use of FFT across all healthcare settings, including hospitals, primary care practices, and mental health services.
The FFT has also been adopted in other countries, such as Australia and the United States, as a means of capturing patient feedback and driving quality improvement efforts.
The FFT follows the same scoring and categorization system as NPS, with patients classified as Promoters, Passives, or Detractors based on their likelihood to recommend the healthcare service. Healthcare organizations can use FFT scores to track patient satisfaction over time, identify areas for improvement, and compare performance across different units or services.
Benefits and limitations of using NPS/FFT in health care
The use of NPS and FFT in healthcare settings offers several potential benefits:
- Simplicity and ease of use: The single-question format of NPS/FFT makes it easy for patients to provide feedback and for healthcare organizations to administer and interpret the results.
- Benchmarking and comparison: NPS/FFT scores allow healthcare organizations to compare their performance against peers and track progress over time.
- Identification of improvement opportunities: By analysing NPS/FFT scores and patient comments, healthcare organizations can identify specific areas for improvement and prioritize quality initiatives.
- Promotion of patient-centred care: The use of NPS/FFT demonstrates a commitment to patient feedback and can help foster a culture of patient-centeredness within healthcare organizations.
However, there are also limitations and challenges associated with using NPS/FFT in healthcare:
- Limited scope: NPS/FFT provides a narrow view of patient experience and may not capture the full range of factors influencing patient satisfaction and loyalty.
- Response bias: NPS/FFT scores may be influenced by factors such as survey timing, mode of administration, and patient characteristics, potentially leading to biased results.
- Lack of actionable insights: While NPS/FFT can identify areas for improvement, it may not provide specific guidance on how to address identified issues.
- Overemphasis on a single metric: Healthcare organizations may place undue emphasis on NPS/FFT scores at the expense of other important quality and safety measures.
Despite these limitations, the NPS and FFT remain valuable tools for healthcare organizations seeking to measure and improve patient satisfaction and loyalty. When used in conjunction with other patient experience metrics and quality improvement strategies, NPS/FFT can contribute to the delivery of high-quality, patient-centred care.
Implementing NPS/FFT in Health Care Settings
Planning and preparation
Setting objectives and defining the scope
Before implementing NPS/FFT in a healthcare setting, it is crucial to set clear objectives and define the scope of the initiative. This involves determining the specific goals of measuring patient satisfaction and loyalty, such as identifying areas for improvement, benchmarking performance, or monitoring the impact of quality improvement efforts. The scope should specify which healthcare services, units, or patient populations will be included in the NPS/FFT data collection process.
Engaging staff and stakeholders
Successful implementation of NPS/FFT requires the engagement and support of various stakeholders, including healthcare providers, administrators, and patient representatives. Engaging staff early in the planning process can help foster a sense of ownership and commitment to the initiative. This may involve providing training on the purpose and methodology of NPS/FFT, addressing concerns or reservations, and highlighting the potential benefits for patient care and organizational performance.
Data collection methods and tools
Survey design and administration
The design and administration of NPS/FFT surveys should be carefully considered to ensure the validity and reliability of the data collected.
This includes determining the appropriate timing and frequency of surveys, choosing the mode of administration (e.g., paper-based, electronic, or telephone), and developing clear and concise survey instructions.
It is also important to consider the language and literacy levels of the patient population and where necessary use translation services to offer surveys in multiple languages when necessary.
Combining NPS/FFT with other feedback mechanisms
While NPS/FFT provides a valuable overall measure of patient satisfaction and loyalty, it may not capture the full range of patient experiences and opinions.
Therefore, healthcare organizations should consider combining NPS/FFT with other feedback mechanisms, such as more detailed patient experience surveys, qualitative interviews, or focus groups.
This multi-faceted approach can provide a more comprehensive understanding of patient perspectives and help identify specific areas for improvement.
Analysing and interpreting NPS/FFT data
Calculating and benchmarking scores
NPS/FFT should be tracked over time to monitor progress and can also be benchmarked against other healthcare organizations or industry standards.
However, it is important to interpret NPS/FFT scores in the context of the specific healthcare setting and patient population, as scores may vary widely across different contexts.
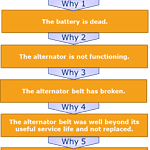
Identifying drivers of patient experience and satisfaction
In addition to calculating the overall NPS/FFT score, healthcare organizations should analyse the data to identify specific drivers of patient experience and satisfaction. This may involve examining the distribution of Promoter, Passive, and Detractor responses, as well as analysing patient comments and feedback to identify common themes or issues. By understanding the factors that influence patient loyalty and satisfaction, healthcare organizations can prioritize improvement efforts and allocate resources more effectively.
Acting on NPS/FFT feedback
Developing and implementing improvement strategies
The ultimate goal of collecting NPS/FFT feedback is to drive improvements in patient care and experience. Based on the insights gathered from NPS/FFT data analysis, healthcare organizations should develop targeted improvement strategies. This may involve changes to clinical processes, staff training and development, facility upgrades, or communication practices. Improvement efforts should be prioritized based on their potential impact on patient experience and alignment with organizational goals and resources.
Communicating results and actions to patients and staff
To demonstrate a commitment to patient feedback and continuous improvement, healthcare organizations should communicate NPS/FFT results and subsequent actions to both patients and staff. This may involve sharing summary reports, highlighting success stories, or acknowledging areas for improvement. Communicating results and actions can help build trust and engagement among patients and staff, and reinforce the importance of patient experience as a key driver of quality care.
Lessons learned and best practices for using NPS/FFT effectively
Secure leadership support and engagement
Successful implementation of NPS/FFT requires the support and engagement of senior leadership. Healthcare executives should champion the importance of patient feedback and allocate sufficient resources for data collection, analysis, and improvement efforts. Leadership should also communicate the value of NPS/FFT to staff and encourage their participation in the feedback process.
Integrate NPS/FFT with other patient experience metrics
While NPS/FFT provides a valuable overall measure of patient satisfaction and loyalty, it should be used in conjunction with other patient experience metrics to gain a comprehensive understanding of performance. This may include more detailed patient experience surveys, patient complaints and compliments, and clinical quality measures. Integrating NPS/FFT with other metrics can help identify specific areas for improvement and prioritize action steps.
Use NPS/FFT data to drive continuous improvement
Collecting NPS/FFT feedback is only the first step; healthcare organizations must use the insights gained to drive continuous improvement in patient care and experience. This requires a systematic approach to data analysis, action planning, and implementation. Healthcare organizations should establish regular review processes to discuss NPS/FFT results, identify improvement opportunities, and monitor progress over time.
Communicate results and actions to patients and staff
Transparency and communication are key to building trust and engagement in the NPS/FFT process. Healthcare organizations should share NPS/FFT results and subsequent actions with both patients and staff. This may involve publishing summary reports, highlighting success stories, or acknowledging areas for improvement. Communicating results and actions demonstrates a commitment to patient feedback and can help sustain momentum for ongoing improvement efforts.
Continuously refine and adapt the NPS/FFT process
Implementing NPS/FFT in healthcare settings is an iterative process that requires ongoing refinement and adaptation. Healthcare organizations should continuously monitor the effectiveness of their NPS/FFT process and make adjustments as needed. This may involve modifying survey questions, changing data collection methods, or adjusting improvement strategies based on patient feedback and changing organizational priorities. By learning from successful NPS/FFT implementations and adopting best practices, healthcare organizations can effectively leverage patient feedback to drive improvements in patient experience, satisfaction, and loyalty.
Integrating NPS/FFT with Other Patient Experience Measures
The role of NPS/FFT within a comprehensive patient experience measurement framework
While NPS/FFT provides a valuable overall measure of patient satisfaction and loyalty, it should be viewed as one component of a comprehensive patient experience measurement framework. A holistic approach to measuring patient experience incorporates multiple data sources and feedback mechanisms to capture the full range of patient perspectives and experiences.
In addition to NPS/FFT, a comprehensive patient experience measurement framework may include:
- Detailed patient experience surveys: These surveys delve deeper into specific aspects of the patient experience, such as communication with healthcare providers, care coordination, and the physical environment of care. Surveys may be administered through various channels, such as mail, phone, or online, and can provide more granular insights into areas for improvement.
- Patient complaints and compliments: Monitoring and analysing patient complaints and compliments can provide valuable real-time feedback on patient experiences. This data can help identify emerging issues or trends and guide immediate improvement efforts.
- Social media monitoring: With the growing use of social media platforms, patients increasingly share their healthcare experiences online. Monitoring social media mentions and sentiment can provide additional insights into patient perceptions and experiences.
- Patient focus groups and interviews: Qualitative research methods, such as focus groups and interviews, can provide rich, in-depth insights into patient experiences and perspectives. These methods can help uncover the “why” behind NPS/FFT scores and identify areas for improvement that may not be captured through quantitative measures.
- Patient journey mapping: Mapping the patient journey from initial contact through post-discharge follow-up can help identify key touchpoints and moments of truth that influence patient experience and satisfaction. This process can help prioritize improvement efforts and ensure a seamless, patient-centred experience across the continuum of care. By integrating NPS/FFT with other patient experience measures, healthcare organizations can gain a more comprehensive and nuanced understanding of patient perspectives and experiences. This holistic approach can help prioritize improvement efforts, track progress over time, and ensure that patient feedback drives meaningful changes in care delivery.
Combining NPS/FFT with other feedback tools and data sources
To maximize the value of NPS/FFT, healthcare organizations should consider combining it with other feedback tools and data sources. This approach can provide a more complete picture of patient experience and help identify areas for improvement that may not be captured through NPS/FFT alone.
Some examples of how NPS/FFT can be combined with other feedback tools and data sources include:
- Combining NPS/FFT with patient experience surveys: By including the NPS/FFT question as part of a broader patient experience survey, healthcare organizations can collect both overall loyalty metrics and more detailed feedback on specific aspects of care. This approach can help identify the key drivers of patient satisfaction and loyalty and guide targeted improvement efforts.
- Integrating NPS/FFT with patient complaints and compliments: Analysing NPS/FFT scores in conjunction with patient complaints and compliments can provide a more balanced view of patient experiences. This approach can help identify areas where patient feedback is consistent across multiple channels and highlight discrepancies that may require further investigation.
- Linking NPS/FFT with clinical quality measures: Integrating NPS/FFT data with clinical quality measures, such as readmission rates, infection rates, and patient outcomes, can provide insights into the relationship between patient experience and clinical performance. This approach can help prioritize improvement efforts that have the greatest potential impact on both patient satisfaction and clinical quality.
- Combining NPS/FFT with employee engagement metrics: Patient experience is closely linked to employee engagement and satisfaction. By analysing NPS/FFT scores in conjunction with employee engagement metrics, healthcare organizations can identify areas where staff satisfaction may be impacting patient experience and develop targeted interventions to support both patients and employees. By combining NPS/FFT with other feedback tools and data sources, healthcare organizations can develop a more comprehensive and actionable approach to measuring and improving patient experience. This integrated approach can help break down silos between different data sources, identify key themes and trends, and drive system-wide improvements in care delivery.
Future Directions and Challenges
Emerging trends and innovations in patient experience measurement
As healthcare organizations continue to prioritize patient experience, new trends and innovations are emerging in the field of patient experience measurement. These developments aim to address the limitations of traditional feedback mechanisms and provide more comprehensive, real-time insights into patient perspectives and experiences.
Some emerging trends and innovations in patient experience measurement include:
- Real-time feedback: Advances in technology are enabling healthcare organizations to collect and analyze patient feedback in real-time. This approach allows for immediate identification of issues and concerns, enabling rapid response and problem resolution. Real-time feedback can be collected through various channels, such as mobile apps, SMS, and in-room tablets.
- Artificial intelligence (AI) and natural language processing (NLP): AI and NLP technologies are being used to analyze large volumes of unstructured patient feedback data, such as open-ended survey responses and social media comments. These technologies can help identify key themes and sentiments, providing deeper insights into patient experiences and enabling more targeted improvement efforts.
- Personalized feedback: Personalized feedback mechanisms are being developed to tailor the patient experience measurement process to individual patient preferences and needs. This approach may involve customizing survey questions based on patient demographics, health conditions, or previous feedback history. Personalized feedback can help increase patient engagement and provide more relevant insights for improvement efforts.
- Patient-reported outcome measures (PROMs): PROMs are standardized, validated questionnaires that capture patients’ self-reported health status, functional abilities, and quality of life. Integrating PROMs into patient experience measurement can provide a more comprehensive view of patient outcomes and experiences, enabling healthcare organizations to better understand the impact of care on patients’ lives.
- Gamification and incentives: Some healthcare organizations are exploring the use of gamification and incentives to increase patient engagement in the feedback process. This approach may involve offering rewards or recognition for completing surveys, participating in focus groups, or providing feedback through other channels. Gamification can help make the feedback process more engaging and enjoyable for patients, potentially increasing response rates and data quality.
Addressing challenges and limitations of NPS/FFT in health care settings
While NPS/FFT has shown promise as a patient experience measurement tool in healthcare settings, there are several challenges and limitations that must be addressed to ensure its effectiveness and validity.
Some challenges and limitations of NPS/FFT in healthcare settings include:
- Response bias: NPS/FFT scores may be influenced by factors such as survey timing, mode of administration, and patient characteristics. For example, patients who are more satisfied with their care may be more likely to respond to surveys, leading to inflated scores. Healthcare organizations must be aware of potential response biases and take steps to mitigate them, such as using multiple survey modes and ensuring representative sampling.
- Cultural and linguistic barriers: NPS/FFT questions may not translate well across different cultures and languages, leading to misinterpretation or inaccurate responses. Healthcare organizations must ensure that NPS/FFT questions are culturally and linguistically appropriate for their patient populations and provide translation services as needed.
- Lack of actionable insights: While NPS/FFT provides an overall measure of patient loyalty and satisfaction, it may not provide specific insights into areas for improvement. Healthcare organizations must combine NPS/FFT with other feedback mechanisms and data sources to gain a more comprehensive understanding of patient experiences and identify actionable improvement opportunities.
- Overemphasis on a single metric: Healthcare organizations may place undue emphasis on NPS/FFT scores at the expense of other important measures of patient experience and clinical quality. It is important to view NPS/FFT as one component of a broader patient experience measurement framework and to balance its use with other metrics and data sources.
- Resistance to change: Implementing NPS/FFT and acting on patient feedback may require significant changes to organizational culture, processes, and workflows. Healthcare organizations may face resistance from staff who are uncomfortable with change or who feel that patient feedback is not relevant to their work. Effective change management strategies, such as communication, training, and leadership support, are essential for overcoming resistance and ensuring the success of NPS/FFT initiatives.
References
Kash, B., & McKahan, M. (2017). The Evolution of Measuring Patient Satisfaction. Journal of Primary Health Care and General Practice.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013 Jan 17;368(3):201-3. doi: 10.1056/NEJMp1211775. Epub 2012 Dec 26. PMID: 23268647.
Wolf JA, Niederhauser V, Marshburn D, LaVela SL. Defining Patient Experience. Patient Experience
Journal. 2014; 1(1):7-19. doi: 10.35680/2372-0247.1004.
LaVela SL, Gallan AS. Evaluation and measurement of patient experience. Patient Experience Journal. 2014; 1(1):28-36. doi: 10.35680/2372-0247.1003.